Care and Outcomes in Pediatric Convulsive Status Epilepticus
Abstract number :
3.341
Submission category :
Late Breakers
Year :
2013
Submission ID :
1867588
Source :
www.aesnet.org
Presentation date :
12/7/2013 12:00:00 AM
Published date :
Dec 5, 2013, 06:00 AM
Authors :
D. V. Jillella, J. Zelener, J. Klehm, S. An, N. E. Kadish, I. S nchez Fern ndez, T. Loddenkemper
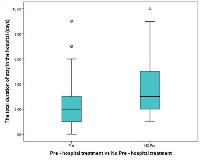
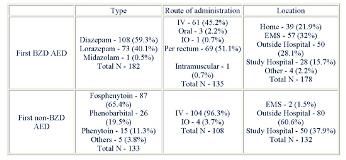
Rationale: Convulsive status epilepticus is one of the most frequent neurologic emergencies in the pediatric population. The aim of this study is to describe the care of pediatric patients with generalized convulsive status epilepticus and their outcomes.Methods: We retrospectively identified pediatric patients who were admitted to the neurology department of a reference pediatric hospital with a diagnosis of seizures or status epilepticus. We included patients who: 1) were 1 month - 21 years of age, 2) had at least one episode of generalized convulsive status epilepticus (GCSE), 3) lasting 30 minutes, 4) in the 6-year period between January 1st 2005 and December 31st 2010. We considered patients with out-of-hospital GCSE onset and excluded patients who presented with GCSE during hospital admission. When several episodes of GCSE occurred in the same patient, only the first episode was analyzed.Results: A total of 185 patients (98 males) with a median (p25-p75) age at onset of 3.5 (1.4 7.2) years were enrolled. The first antiepileptic drug (AED) was a Benzodiazepine (BZD) in 178 (96.7%) patients: diazepam in 108 (60.7%) and lorazepam in 70 (39.3%). A non-benzodiazepine AED was administered in 133 (72.2%) patients: fosphenytoin in 87 (65.4%), phenobarbital in 26 (19.5%), phenytoin in 15 (11.3%) and others in 5 (3.8%). In 91 (49.7%) patients, treatment was initiated prior to the hospital arrival and was initiated at the hospital in 93 (50.3%). The median (p25-p75) duration of hospital stay was shorter in patients with pre-hospital treatment compared to those without pre-hospital treatment [2 (1-3) days versus 3 (2-5) days; Wilcoxon rank-sum test p = 0.007]. 84 patients (45.4%) were admitted to the ICU: 39 (39.1%) patients with pre-hospital treatment and 48 (51.6%) with no pre-hospital treatment (Pearson Chi-square p = 0.08) (Figure 1). Hypotension, as clinically assessed, was seen in 14 (7.6%) patients and 8 (57%) needed the use of a vasopressor agent. Hypotension was seen in 2 patients in whom a single BZD was used and in 12 patients in whom 2 or more BZDs were used (Fisher s exact test p = 0.03). EEG was performed in 100 (54.1%) patients and EEG abnormalities were found in 82 (82%) and Electrographic SE was seen in 8 (8%) patients. A CT was performed in 108 (58.4%) patients and 48 (44.4%) had abnormalities, including a: baseline abnormality in 29 (26.9%) and new abnormality in 19 (17.6%). MRI of the brain was performed in 50 (27%) patients and 28 (56%) had abnormalities, including a: baseline abnormality in 8 (16 %) and a new abnormality in 20 (40 %). One patient (1.6%) died during admission and the cause of death was determined to be septic shock.Conclusions: Patients who received treatment before hospital arrival had a shorter duration of hospital stay when compared to patients who did not receive any treatment before hospital arrival. There was also a tendency towards lower rate of ICU admissions in patients who received pre-hospital treatment when compared to those who did not receive any pre-hospital treatment. Results may inform improved status epilepticus treatment and prevention strategies.