Efficacy and Safety of Rapid Cycling Vagus Nerve Stimulation in Children With Intractable Epilepsy, Especially Myoclonic Seizures
Abstract number :
1.224
Submission category :
4. Clinical Epilepsy / 4C. Clinical Treatments
Year :
2018
Submission ID :
498906
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Husam Kayyali, King Faisal Specialist Hospital and Research Centre; Kyle Smith, University of Kansas; Erin Fecske, Children's Mercy Hospital; Ahmed Elbermawy, University of Missouri at Kansas City; Lalit Bansal, Children's Mercy Hospital; Megan Gustafson,
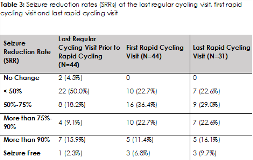
Rationale: Vagus nerve stimulation (VNS) is an effective therapy for pharmacoresistant epilepsy. Nevertheless, information is lacking regarding the optimization of stimulation parameters to improve patient outcomes. The objective of this study is to examine the safety and efficacy of rapid duty cycle VNS (defined as off time =1.1 minute keeping duty cycle Methods: This is a retrospective review of 50 patients with 45 having myoclonic seizures (1-17 years) with intractable epilepsy who were treated with VNS between 2010 to 2015 at a single pediatric epilepsy center. Safety and tolerability, data were aggregated across all patient visits to determine frequency of side effect or adverse event between differing duty cycles. Also, we compared seizure reduction rates (SRR) for each patient at 1) last regular duty cycle visit; 2) first rapid duty cycle visit; and 3) last recorded rapid duty cycle visit. Results: Rapid duty cycle was well tolerated with no adverse events reported in 96.6% of patient encounters. At the last visit prior to switching to rapid cycling, 20 patients (44.5%) were showing response to VNS (SRRs =50%). This number increased to (77.3%) after switching to rapid cycling, and remained at (77.4%) at the last rapid cycling visit. Fifteen patients (34.1%) became responders to VNS after they switched to rapid cycling, another 19 (43.2%) maintained their response with mostly improved SRRs. There were only few instances where responders became non-responders after they switched to rapid cycling VNS. Conclusions: Rapid cycling VNS is probably safe and well tolerated especially in patients with myoclonic seizures. It may also be more efficacious than regular cycling VNS in some patients. This study highlights the necessity of prospective, long-term, double-blinded studies for understanding the advantages of this VNS modality. Funding: Internal funding
.tmb-.png?Culture=en&sfvrsn=dbf89e63_0)