ANTERIOR TEMPORAL LOBECTOMY VERSUS SELECTIVE AMYGDALOHIPPOCAMPECTOMY FOR TEMPORAL LOBE EPILEPSY DUE TO HIPPOCAMPAL SCLEROSIS: SEIZURE OUTCOME OVER THE YEARS
Abstract number :
2.420
Submission category :
Year :
2004
Submission ID :
4869
Source :
www.aesnet.org
Presentation date :
12/2/2004 12:00:00 AM
Published date :
Dec 1, 2004, 06:00 AM
Authors :
1Ney Azambuja, 1,2Eliseu Paglioli, 1Andre Palmini, 1Jaderson Costa, 1Mirna Portuguez, and Jose Martinez
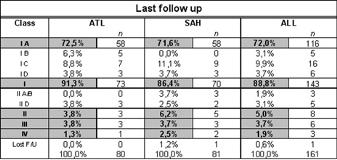
The increasing ability to visualize the sclerotic hippocampus by magnetic resonance imaging (MRI) and the evolving knowledge about the pathogenic bases of mesial temporal lobe epilepsy due to hippocampal sclerosis (MTLE/HS) have raised questions about the best surgical approach to treat these patients. We compare two groups patients with MRI and pathology-confirmed MTLE/HS, who were uniformly evaluated, presented a very homogeneous clinical picture, and were operated by the same surgeon through either an anterior temporal lobectomy (ATL) or a selective amygdalohippocampectomy (SAH). Surgical outcome in regard to seizure control was analyzed for 161 consecutive patients operated in Porto Alegre for MTLE/HS, from January 1992 to March 2002. These were drawn from a total of 569 patients operated for intractable epilepsy in the same period, 285 of whom in the temporal lobe. Eighty patients had an ATL (Spencer technique) and the other 81 had a SAH, in which mesial structures were removed according to the technique originally described by Niemeyer. Data is presented in regard to the outcome at the last updated visit and also as a Kaplan_Meyer survival analysis in each Engel[rsquo]s outcome class. After a mean follow up of 5.8 years (range, 24 - 132), 116 patients (72.0%) had been completely seizure free since surgery (class IA), 143 (88.8 %) were in outcome class I, and 151 (93.7%) were either in outcome classes I or II. Fifty-eight (72.5%) of the 80 ATL patients (mean follow up of 7.5 years) and also 58 (71.6%) of the 81 patients undergoing a SAH (mean follow up of 4.2 years) continued to be completely seizure free since surgery (outcome class IA). Tests for equality of survival distributions comparing both techniques in outcome classes IA, I, and I or II were not significantly different at any point in time. Only one of the 161 patients (0.6%) with MTLE/HS was lost to follow up. Patients were followed for two to 11 years, with a mean of 5.04.[figure1] Surgical results for TLE/HS are stable over time and highly satisfactory, irrespective of the chosen technique. These highly satisfactory results can be achieved with a limited incision of the temporal neocortex. Since both (ATL and SAH) lead to extremely satisfactory results, it is likely that a neocortex-sparing technique (SAH) should be preferred.