New Onset Epilepsy in New Onset Seizure Clinic (NOSc)
Abstract number :
2.414
Submission category :
16. Epidemiology
Year :
2018
Submission ID :
502705
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Seunghyo Kim, Emory University; Ton Degrauw, Emory University; Kristen Hass, Children's Healthcare of Atlanta; Anne T. Berg, Ann & Robert H. Lurie Children's Hospital of Chicago; and Sookyong Koh, Emory University
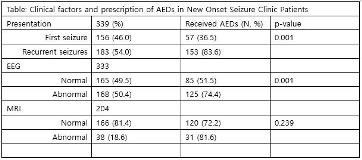
Rationale: We sought to evaluate clinical and demographic features of children presenting with unprovoked seizures at a regional New Onset Seizure clinic (NOSc). Methods: Retrospective chart review of consecutive patients evaluated in the NOSc at Children’s Healthcare of Atlanta from 9/22/2015 to 9/16/2016. Results: Of 494 children, 156 (32%) had a first unprovoked seizure (1SZ) and 183 (37%) recurrent seizures (RecSZ). Others had febrile seizures (N=22, 4%), provoked seizures (N=11, 2%), established epilepsy (N=16, 3%), and breakthrough seizures after stopping anti-seizure medications (ASM, N=3, <1%); 102 (19%) had nonepileptic events. Of 339 patients with newly-presenting unprovoked seizures, 180 (53%) were African American, 121 (36%) Caucasian; 157 (46%) were girls. The average age at first seizure was 7.4 ±4.7 years and at the first NOS visit, 7.9 ± 4.7 years. Patients were referred from the emergency department (ED, N=248, 73%) or primary care providers (N=87, 26%). Presenting seizure types included tonic-clonic (N=184, 54%), focal motor (N=65, 19%), staring/behavioral arrest (N=38, 11%), absence (N=22, 7%), and others (N=30, 9%). Syndromic diagnoses were made in 79 (23%) including BECTS, (N=28), CAE (N=20), JME (N=8), MTLE ( N=5), JAE (N=20); and other syndromes (N=14). Average time from first seizure to NOS visit was 6.7 months; those with staring spells (8.4 months) and absence seizures (8.7 months) took substantially longer. Comorbidities identified included developmental delay (N=71, 21%,), learning disability (N=64, 19%), autism (N=21, 6%), ADHD (N=19, 6%), and cerebral palsy (N=8, 2%). EEGs performed in 333 (98%) identified epileptic discharges in 154 (45%). Brain MRI, performed in 204 (60%), identified etiologically relevant abnormalities in 38 (19%). ASMs were prescribed in 210/339 (62%) of children. ASMs were prescribed more often in children with RecSZ than 1SZ (p=0.001) and abnormal versus normal EEG findings (p=0.001), but not those with abnormal MRI findings (p=0.24) (Table). Levetiracetam was the commonly started ASM in the ED (N=52, 79%). Choice of ASMs initiated in the NOSc was more variable including levetiracetam (35%) oxcarbazepine (24%) lamotrigine (17%), and valproic acid (12%). 47 (30%) children who presented with a 1SZ had a recurrence over the following year. Children with abnormal EEGs (p=0.04), seizures arising from sleep (p=0.005) were at greatest risk for recurrence. Conclusions: Of children evaluated in a large regional NOSc, most have newly-presenting seizures and majority (>