Temporal Lobectomy Without Amygdalohippocampectomy in a Pediatric Population: A Case Series
Abstract number :
1.353
Submission category :
9. Surgery / 9B. Pediatrics
Year :
2018
Submission ID :
506964
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Thuy-anh Vu, Children's National Medical Center; Kathryn Havens, Children's National Medical Center; Chima Oluigbo, Children's National Medical Center; and William Gaillard, Children's National Medical Center
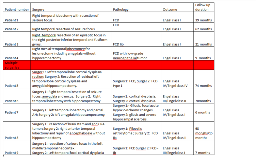
Rationale: It is standard to do temporal lobectomy with amygdalohippocampectomy (AH) for temporal lobe epilepsy especially when there is evidence of mesial temporal sclerosis. However due to various reasons we have several patients where AH was not pursued with a temporal lobectomy. We noted that a few of these patients returned for additional epilepsy surgery. We examined our database for patients with temporal lobectomy without AH to examine outcomes. Methods: We retrospectively identified patient who underwent surgical intervention from October 2011 to June 2017 with at least 6 month follow-up postop. The database was queried for demographics, MRI, pathology, and Engel outcome. Results: We have nine patients with medically refractory epilepsy with temporal lobectomy without complete amygdalohippocampectomy or without hippocampectomy. Four of these patients (44.4%) had a single surgery, and five (55.6%) had two surgeries. Of the four patients with single surgery, all four are seizure free, Engel class I, with 9-62 months of follow up. Pathology for three of the patients was focal cortical dysplasia and one had focal cortical dysplasia with low grade neuroepithelial tumor.Five of the patients without AH on their first surgery had Engel class IV outcomes.Of the five patients with more than one surgery, three eventually had a complete amygdalohippocampectomy. One continued with class IV outcomes, one has class II outcome, and one has class I outcome – the latter two had short follow up from second surgery. Pathology respectively was focal cortical dysplasia for the first two and gliosis and hippocampal sclerosis for the third patient.Two of the five patients with more than one surgery did not have an AH and did improve to class II outcomes with their second surgery. Pathology for both were focal cortical dysplasia, with one with a prior pilocytic astrocytoma. Conclusions: Although the majority of patients with temporal lobectomies for refractory epilepsy have amygdalohippocampectomy, there are situations where it is not done. We have several patients in our series that have had successful temporal lobectomy without AH. Those that had poor outcomes had additional surgeries with and without AH, with the majority having improved outcomes. Each patient must be individually evaluated, but there is hope with additional surgeries to improve outcomes if the first surgery is not successful. Funding: None