September 10, 2018
Seema Verma
Administrator
Centers for Medicare & Medicaid Services,
Department of Health and Human Services,
Attention: CMS-1693-P
Mail Stop C4-26-05
7500 Security Boulevard
Baltimore, Maryland 21244-1850
SUBMITTED ELECTRONICALLY VIA http://www.regulations.gov
Re: Medicare Program; Revisions to Payment Policies Under the Physician Fee Schedule and Other
Revisions to Part B for CY 2019; (CMS–1693–P)
Dear Administrator Verma:
The National Association of Epilepsy Centers (NAEC), the American Clinical Neurophysiology Society (ACNS), and the American Epilepsy Society (AES) are pleased to offer comments on the proposed rule outlining revisions to the Medicare Physician Fee Schedule
(PFS) for 2019. Our comments focus on:
1. Proposals Related to Evaluation & Management Visits - Documentation and Payment Policies
2. Public Comment Solicitation on Eliminating the Prohibition on Billing Same-Day Visits by Practitioners of the Same Group and Specialty
3. Teaching Physician Documentation Requirements for Evaluation and Management Services
4. Proposed RVUs for Revised and New CPT Codes for Neurostimulators, and ECoG services
Background
NAEC is an organization of 240 specialized epilepsy centers in the United States dedicated to developing standards of care and promoting their adoption by epilepsy centers through its accreditation program. NAEC pursues an active agenda,
educating public and private insurers, policymakers, and government officials about the complexities of and need for patient access to specialized epilepsy services.
ACNS is the major professional organization in the United States devoted to the establishment and maintenance of standards of professional excellence in clinical neurophysiology in the practice of neurology, neurosurgery and psychiatry. ACNS members utilize
neurophysiology techniques in the diagnosis and management of patients with disorders of the nervous system and in research examining the function of the nervous system in health and disease. ACNS is seated in the AMA House of Delegates and is part
of the North America Chapter of the International Federation of Clinical Neurophysiology (IFCN).
Founded in 1946, the American Epilepsy Society (AES) is the national medical and scientific society whose members are dedicated to advancing research and education for preventing, treating and curing epilepsy. With more than 4,000 members, AES is an inclusive
global forum where professionals from academia, private practice, not-for-profit, government and industry combine efforts to eradicate epilepsy and its consequences.
As national subspecialty organizations, whose members are dedicated to the diagnosis and management of patients with epilepsy, our comments will provide CMS with the expected impact of the proposed rule on the complex care provided by our members to patients
with intractable epilepsy. Epilepsy is a serious chronic condition with unpredictable life-threatening exacerbations. Many patients are relatively easy to diagnose and a single medication will be effective in controlling seizures without causing side-effects.
Unfortunately 25 – 30% of patients living with epilepsy have intractable or refractory seizures and often multiple co-morbidities. For many of these patients it takes many years to accurately diagnose and effectively treat their epilepsy. We
believe Medicare includes a significant number of patients with intractable epilepsy, as many are eligible for benefits due to their disability rather than their age.
Many patients with intractable epilepsy are treated by epileptologists (neurologists specializing in epilepsy) and are seen at specialized epilepsy centers, which utilize a multi-disciplinary approach to provide the highest level of tertiary care. This
often includes visits with epileptologists, neurosurgeons, mental health professionals, neuropsychologists, nurse specialists and other team members. Through this team approach, patients are evaluated on both an outpatient and inpatient basis to determine
what type of seizures are occurring, which part of the brain is affected, and what treatments may be effective. This high level of evaluation identifies patients who are good candidates for surgery, which can be a means to cure their epilepsy.
Evaluation & Management Visits – Documentation and Payment Proposals
We commend CMS for recognizing the documentation burden associated with the existing evaluation &
management (E/M) codes and appreciate the agency’s recognition in the proposed rule that the existing outpatient E/M services and their documentation requirements do not accurately reflect current medical practice nor do they distinguish the
level of service provided or the resources utilized.
While our organizations support many of the proposed changes to the documentation requirements for
reporting E/M services, we oppose the consolidation of level 2 - 5 E/M services into a single payment
rate. The consolidation of E/M visits will directly impact patient access to and the quality of epilepsy care. Patients are referred to epilepsy specialists or an epilepsy center when the first line of treatments are not effective. Patients with
intractable epilepsy have visits dominated by the explanation of the diagnostic tests and treatments to enable them to make the best decisions regarding their care. Time for education and counseling is especially important for patients when medications
are not effective and brain surgery, though risky, is a better option. It is through the higher level E/M visits that the physician develops the relationship with the patient to get them to overcome their fears and select a more invasive, but better
treatment option. Providing high quality care and achieving the best outcomes requires the face-to-face time to thoroughly explain the issues and answer the questions of the patient and their family members.
The proposed changes to E/M reimbursement are likely to directly reduce the opportunity to provide this level of care, since physicians will be encouraged to spend less time in each visit as they strive to fit more patients into their schedules. Or, patients
and their caregivers may be forced to return for an additional visit at additional financial and time costs. Additionally, patients will either be overpaying or underpaying their co-payments for these services since their share will no longer correlate
to their service level.
Despite CMS’ proposed add-on codes for neurology services and prolonged services to soften the payment reduction (discussed in more detail below), we believe the net effect of the changes will be a reduction in payment for neurologists specializing
in epilepsy care. For this reason our organizations oppose the proposed E/M payment policies and ask that CMS work with stakeholders to develop alternative approaches to E/M payment and documentation requirements that can be implemented in 2020.
Consolidation of E/M Visits to Single Payment Rate
Our members typically utilize level 4 and 5 E/M codes for outpatient services, with most new patient visits coded at a level 5 and follow-up visits with established patients coded as level
3 or 4. For this reason, epileptologists will be disproportionately harmed by this proposal. CMS’s impact tables in the proposed rule state that neurology will face a negative 2 percent reduction, while an analysis conducted by the American
Medical Association (AMA) attached to this lettershows that neurology payments will decrease by 5 percent. It is not clear what is causing the differences in the analyses, but we believe that since epileptologists provide a high volume of higher-level
E/M services, the negative impact for our members will likely be much more significant.
Level 4 and 5 visits are the only way to reflect the cognitive intensity required to care for the most complicated, challenging, and vulnerable patients with epilepsy that our members treat. By consolidating these E/M services, there will be no way to
account for the higher level of care and complexity of the patients being seen. Since consultation codes have been eliminated, the current E/M coding structure is the only means specialists have to distinguish the complexity of the patients they are
seeing, along with their expertise and experience.
Add-On Code Proposals
To address the reimbursement shortfalls from the consolidation of the E/M services that some specialties would experience, CMS is proposing to create complexity add-ons for primary care of $5 and for certain specialty
care of $13.70. While we appreciate that CMS included neurology as one of the cognitive services that could be reported by the new add-on code, we do not believe that the add-on code will adequately compensate for the intensity and complexity of the
services that epileptologists typically provide. When the specialty add-on code is billed in conjunction with the single payment established patient visit worth $93, this still falls short of the current level 4 reimbursement of $109 and level 5 reimbursement
of $148. This reduction while small will have a significant impact on epilepsy providers.
CMS is also proposing to create a new 30 minute prolonged service code that can be billed with longer visits. We appreciate the agency’s intent to recognize there are circumstances where longer visits are necessary, but it is not clear how this
code would be billed. We ask that CMS provide clarification for the required time for the base E/M code and how much additional time is needed to bill the prolonged service code.
Multiple Procedure Payment Reduction
Our organizations oppose CMS’ proposal to reduce payment by 50 percent for the least expensive procedure or visit that the same physician (or a physician in the same group practice) furnishes on
the same day as a separately identifiable E/M visit, currently identified on the claim using modifier -25. We believe that the AMA Resource Based Relative Value Update Committee (RUC) has already eliminated the overlap in physician work, clinical
staff time, supplies, and equipment for multiple services provided on the same day. If implemented, CMS’ proposed policy will create an additional incentive for physicians to provide procedures separately from office visits at additional time
and expense to patients.
Public Comment Solicitation on Eliminating the Prohibition on Billing Same-Day Visits by Practitioners
of the Same Group and Specialty
Today, Medicare will not pay for two E/M visits billed by a physician (or physician of the same specialty from the same group practice) for the same beneficiary on the same day unless the physician documents that the visits are for unrelated problems.
However, the agency now recognizes that there may be certain instances where this does not make sense and inconveniences patients and has requested comment on this issue.
Our members provide multi-disciplinary care, in which multiple providers collaborate to diagnose and treat a patient’s intractable epilepsy. This highly-specialized care is provided at a limited number of hospitals in the country, meaning that many
patients travel long distances for appointments. Accordingly, patients and caregivers strongly prefer to see all their varied specialists in one day, during one visit. Furthermore, care is enhanced when these providers can meet the patient simultaneously,
to best explain complicated neurological conditions, and the impact various treatments will have on the patient’s brain functions and mental health. The proposed reduction in reimbursement when multiple providers see a patient on the same day
will preclude this multi-disciplinary approach that is a critical element of the superior quality of care provided by highly specialized centers.
Our organizations agree with CMS that this prohibition impedes high-quality patient care. Physicians are increasingly providing team based care and are encouraged by CMS and private payers to do so. P Prohibiting billing two E/M visits on the same day
by practitioners in the same group and specialty undermines the type of collaboration required to deliver team based care effectively. We ask that CMS eliminate this prohibition and reimburse for multiple same-day visits by practitioners of the same
group and specialty.
Teaching Physician Documentation Requirements for Evaluation and Management Services
CMS is responding to feedback that the E/M documentation requirements for visits provided by teaching physicians are burdensome and duplicative of notes already made by residents and other members of the health care team. Our organizations support the
proposed change to allow a physician, resident, or nurse to document the visit and specifically note that the physician was present at the time the service was provided. This proposed change will eliminate duplicative work.
Proposed Values for New and Revised CPT Codes for Neurostimulator Services and Electrocorticography
Our organizations are concerned that CMS is not proposing the RUC-recommended values for neurostimulator CPT codes 95970, 95X83, 95X84, 95X85, and 95X86 and the electrocorticography (ECoG) code 96X00. For each of these services, CMS is proposing reductions
in RVUs in contradiction to the surveys our members participated in and the RUC deliberations and recommendations for these codes. We support the arguments laid out on this topic in the comment letters submitted to CMS by the AMA Relative Value Update
Committee and the American Academy of Neurology and urge CMS to adopt the RUC recommended values for these services.
In addition, we believe CMS has inadvertently not assigned non-facility PE RVUs for the new CPT code for electrocorticography (96X00 - Electrocorticogram from an implanted brain neurostimulator pulse generator/transmitter, including recording, with interpretation
and written report, up to 30 days) discussed on page 35771 of the Proposed Rule. This code was created to capture the service of the physician reviewing stored electrocorticographic data from an implanted brain neurostimulator such as the RNS
System. While the service is typically performed in the physician office setting, not the facility setting, the RVUs would be the same in both settings. We believe this is a mistake and ask that CMS
assign RVUs for the Non-Facility PE RVUs and the Total Non-Facility RVUs as this service is primarily
performed in the physician office.
Thank you for your consideration of our organizations’ comments. Please contact Ellen Riker, NAEC’s Executive Director, at eriker@dc-crd.com or (202) 484-1100 with any questions or for more information.
Sincerely,
Nathan Fountain, MD
President
National Association of Epilepsy Centers
Tobias Loddenkemper, MD, FACNS
President
American Clinical Neurophysiology Society
Shlomo Shinnar, MD, PhD
President
American Epilepsy Society
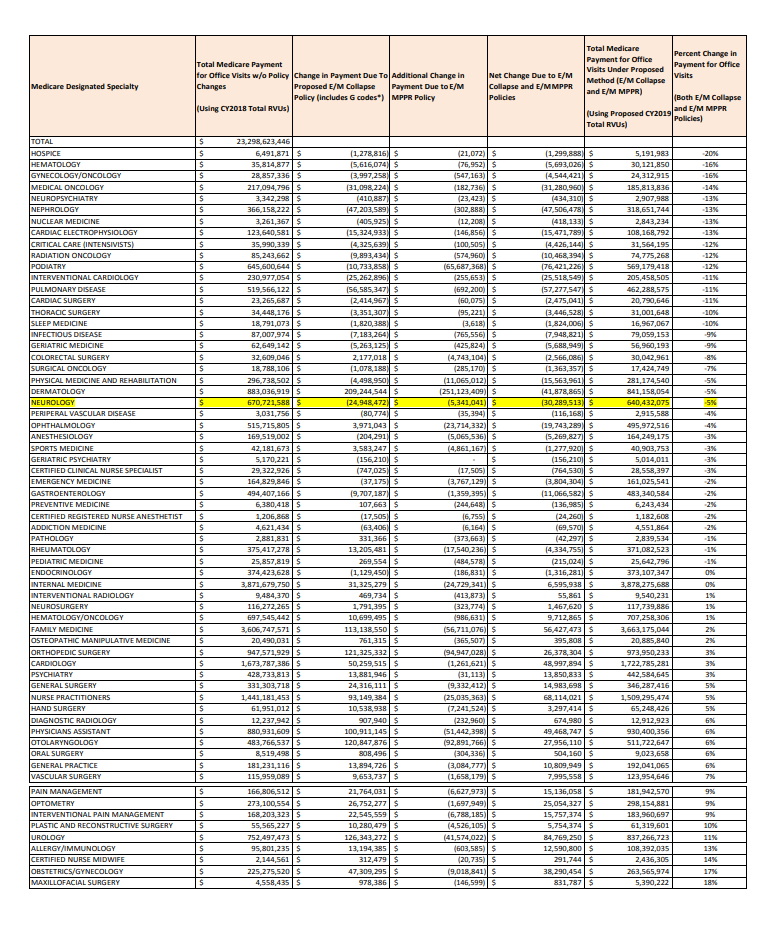
AMA Estimated Impact of CY2019 Evaluation and Management Proposed Policy by Medicare Specialty
*Includes CPT Codes 99201-99215, GCG0X, GCG1X, GPD0X and GPD1X, but does not include GPRO1 - prolonged service Analysis uses Estimated CY2017 Medicare Utilization and CY2019 Medicare CF for both "Current Method" and "Proposed Method"; E/M MPPR Estimate
based on 2016 Medicare Carrier 5% Standard Analytic File Excludes specialties with less than $1 million in CY2017 allowed charges for 99201-99215 or claims with unknown specialty designation