BENIGN ROLANDIC EPILEPSY; NEUROPSYCHOLOGICAL TESTING AND MAGNETIC SOURCE IMAGING ANALYSIS
Abstract number :
2.252
Submission category :
Year :
2004
Submission ID :
2364
Source :
www.aesnet.org
Presentation date :
12/2/2004 12:00:00 AM
Published date :
Dec 1, 2004, 06:00 AM
Authors :
1Freedom F. Perkins, 1Dave F. Clarke, 2Joshua I. Breier, 1Monica M. Chacon, 2Eduardo Castillo, 2David Weers, and 1James W. Wheless
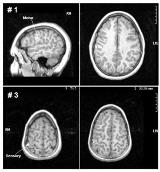
To evaluate children with Benign Rolandic Epilepsy (BRE), a childhood epilepsy characterized by centro-temporal /rolandic spike-wave discharges with infrequent partial seizures which may secondarily generalize. The term [ldquo]benign[rdquo] is incurred because cognitive development has generally been considered unaffected. Recently, some investigators have questioned whether BRE is [ldquo]benign[rdquo] or whether long-term cognitive outcome may be adversely affected. We attempt to better define specific inter-ictal neuropsychological deficits seen in these children and to better localize and lateralize their discharges using magnetoencephalography (MEG)/ magnetic source imaging (MSI). In our institution, we have initiated an ongoing study, identifying children with BRE. These children were all sent for evaluated to our Epilepsy Monitoring Unit (EMU). All children received continuous video-electroencephalography (VEEG) monitoring, brain magnetic resonance imaging (MRI), MEG/MSI and detailed neuropsychological testing. Seven children between the ages of 5 and 11 years have been thus far studied. Varying degrees and patterns of neuropsychological deficit were identified in all subjects. Fine motor dysfunction was seen in the majority, 4/7 patients. Visuomotor integration deficits, dyscalculia and/or expressive language deficits were also identified, thus reaffirming that BRE is not necessarily a benign disorder. MRI was normal in all individuals. Scalp EEG using the International 10-20 System of electrode placement, localized discharges to a fairly wide region including the centro-temporal (perisylivian/perirolandic) areas. MSI derived localization, completed thus far in five patients revealed maximal involvement of the primary motor (M1) and/or primary sensory (S1) cortex.[figure1]Figure 1. MEG-derived localization: Case #1 showed frequent discharges arising from the M1 cortex; and case #3 revealed discharges arising from the S1 cortex. Our study shows a high concordance of specific motor and/or cognitive deficits in BRE. Furthermore, magnetic source imaging shows a higher resolution of dipole localization in the primary motor and sensory areas, when compared with conventional EEG. MEG is a valuable diagnostic tool in the evaluation of children with BRE and may be a valuable tool in predicting deficits found.