Clinical Neurological Features and Electrographic Patterns of Patients With Relapsed or Refractory Large B-Cell Lymphoma Treated with Axicabtagene Ciloleucel at Memorial Sloan Kettering Cancer Center (MSKCC)
Abstract number :
3.134
Submission category :
3. Neurophysiology / 3C. Other Clinical EEG
Year :
2018
Submission ID :
502717
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Alexandra J. Sequeira, Memorial Sloan Kettering Cancer Center; Xi Chen, Memorial Sloan Kettering Cancer Center; Edward K. Avila, Memorial Sloan Kettering Cancer Center; Elena Mead, Memorial Sloan Kettering Cancer Center; Craig S. Sauter, Memorial Sloan Ke
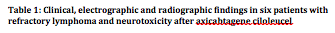
Rationale: CD19-specific chimeric antigen receptor (CAR) T cell therapy is emerging as a promising treatment for hematological malignancies. Axicabtagene ciloleucel is approved to treat adult patients with relapsed or refractory large B-cell lymphoma. Neurotoxicity, also known as CAR-T-cell-related encephalopathy syndrome (CRES), is the second most common adverse effect next to cytokine-release syndrome (CRS) and can occur concurrently or after CRS. Here we describe the clinical neurological features and encephalogram (EEG) patterns of patients with refractory lymphoma treated with axicabtagene ciloleucel at Memorial Sloan Kettering Cancer Center (MSKCC). Methods: We retrospectively analyzed the clinical neurological features and EEG patterns of the first six consecutive patients with refractory lymphoma treated at MSKCC with axicabtagene ciloleucel between February and April 2018. All six patients developed neurotoxicity and all had a long-term video EEG performed. Results: All six patients treated with axicabtagene ciloleucel developed acute neurotoxicity with varying neurotoxicity grades: some with diffuse encephalopathy and others with focal neurological findings (see table 1). Patient ages ranged from 19 to 71. There were 4 males and 2 females. All patients received prophylactic levetiracetam per institutional guidelines and all had a long-term video EEG performed after neurologic symptoms developed. Two patients developed focal neurological findings concerning for focal status epilepticus. One patient had rhythmic right arm movements followed by right arm weakness and the EEG showed focal left lateralized rhythmic delta activity (LRDA) with sharp waves and focal attenuation possibly reflecting a postictal state. The second patient had focal right facial and bilateral eye twitching concerning for focal motor status epilepticus which did not have a scalp correlate. The EEG showed diffuse dysfunction including rhythmic delta activity with frontal predominance and triphasic waves. Both patients had a clinical improvement with escalation of antiepileptic agents (AEDs) with a fosphenytoin loading followed by maintenance dosing. The remaining four patients had EEGs consistent with diffuse cerebral dysfunction and without EEG criteria for seizures. Neuroimaging was performed in all patients and was unrevealing for acute pathology or significant structural pathology. Most patients had resolved encephalopathy and central nervous system symptoms except for a minority who had prolonged symptoms. Conclusions: Axicabtagene ciloleucel can lead to transient diffuse and focal clinical neurological findings of varying severity including focal status epilepticus. EEG can be useful in characterizing the cerebral dysfunction however is limited in detecting epileptic events due to its inability to detect deep cerebral foci. In patients who develop clinical status epilepticus escalation of AEDs may be warranted despite EEG not fulfilling status epilepticus criteria. Further study is needed to determine whether AED escalation can optimize patient outcomes. Funding: None