First Year Experience With Patients in the Post-Acute Symptomatic Seizure (PASS) Clinic
Abstract number :
3.210
Submission category :
4. Clinical Epilepsy / 4C. Clinical Treatments
Year :
2018
Submission ID :
506203
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Stephen Hantus, Cleveland Clinic Foundation; Jessica Fesler, Cleveland Clinic; and Vineet Punia, Cleveland Clinic Foundation
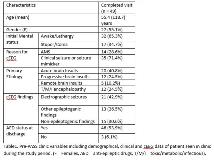
Rationale: : The growing utilization of continuous EEG (cEEG) monitoring has helped identify an increasing number of patients in acute hospital settings with concerning electrographic findings – either clear electrographic seizures or potentially epileptogenic findings predisposing to a higher risk of seizures. Most of these patients are treated with anti-epileptic drugs (AEDs) and invariably discharged on them as well. Previously, we have shown that a large number of these patients remain on AED for prolonged period of time without clear indication for use or benefits. We started a new, dedicated post-acute symptomatic seizure (PASS) clinic at our epilepsy center for the out-patient follow-up of such patients in May 2017. The aim of this study is to describe the clinical characteristics and management experience with patients seen in the PASS clinic in its first year. Methods: Patients qualified to be seen in the PASS clinic if they were adults (=18 years) at the time of cEEG, did not have epilepsy diagnosis at admission, were discharged on at least 1 AED (except Gabapentin). The protocol for PASS clinic visit was a 3 month post-discharge follow-up preceded by a same day, long (75 minutes) routine EEG. For the purpose of this study, we searched our outpatient clinic database for patients who were seen in the PASS clinic from 05/20/2017 to 05/19/2018. We used our prospective cEEG database and EMR to extract relevant clinical variables. Descriptive statistical tools were used to analyze the data. Results: A total of 49 patients [mean age 55.4 (±18.7) years; 55.1% women] were seen in the PASS clinic. Median duration from hospital discharge to PASS clinic visit was 102 (37 – 155) days. A total of 46 (93.9%) patients were discharged on AEDs [14 (28.6%) on =2 AEDs]. Of the 46 patients, Levetiracetam was the most commonly [80.4% patients; median dose 1000 (750 – 1500) mg BID] used AED at discharge, followed by Lacosamide and Valproate (17.4% each). By the time of clinic visit, 9 (18.4%) patients had suffered post-discharge clinical seizures. Routine EEG on the day of clinic visit was performed in 40 (81.6%) patients. It was normal in 15 (25%) and showed potential epileptogenic findings in 5 (12.5%) patients. All 46 patients were on AED at time of clinic visit. AEDs were modified in 24 [52.2%; reduced in 19, increased in 1 and switched to another in 4) patients on clinic visit. A total of 11 (22.5%) patients had more than 1 PASS clinic visit during the study period. Conclusions: We report our first year experience in the PASS clinic - a novel, outpatient model for the longitudinal care of patients managed with AEDs due to cEEG findings during hospitalization. Almost one-fifth of the patients suffered a clinical seizure after hospital discharge, prior to PASS clinic visit. Informed by the outpatient EEG findings, PASS clinic visit impacted the AED therapy in more than 50% patients. We hope to see similar, dedicated clinics at other epilepsy centers in future, which would promote collaborative research and better our understanding of appropriate management and long-term outcomes in these patients. Funding: No funding received.