Improvement in Epilepsy Self-Management Practice and Behaviors Following 12 weeks of Personalized Epilepsy Self-Management Education: Preliminary Results from PAUSE to Learn Your Epilepsy
Abstract number :
3.423
Submission category :
13. Health Services (Delivery of Care, Access to Care, Health Care Models)
Year :
2018
Submission ID :
502165
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Dilip Pandey, University of Illinois at Chicago; Katharine Ozenberger, University of Illinois at Chicago; Jessica Levy, University of Illinois at Chicago; Anna Serafini, University of Illinois at Chicago; Mitra Habibi, University of Illinois at Chicago; W
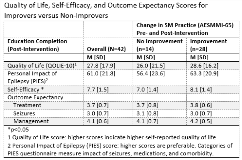
Rationale: Epilepsy is the most common chronic neurologic condition and affects 3.4 million individuals in the U.S. It represents a significant burden to people living with epilepsy (PWE) and their families. Self-management education has been shown to improve quality of life and health outcomes among people living with chronic conditions. There is limited information on how to improve self-management practices in PWE in underserved communities, who have socio-economic, educational, and structural barriers that affect access to self-management education. Moreover, the factors that influence their self-management behaviors following education remain unknown. Methods: The PAUSE to Learn Your Epilepsy evaluates the effectiveness of personalized epilepsy self-management education using mobile technology on improving the lives of adult PWE from underserved populations. A total 42 participants completed on average 12 weeks of personalized self-management intervention through a wireless tablet device. Self-reported demographic characteristics were collected at baseline and tested using chi-square statistics for any statistical differences. Post-intervention assessments of the impact of the personalized self-management education include epilepsy self-management practice (AESMMI-65), self-efficacy, outcome expectancies, personal impact of epilepsy (PIES), and quality of life (QOLIE-10). Participants were considered to have improved in their self-management practice and skills if they had a positive difference between pre- and post-intervention scores. Differences in assessment scores between non-improvers and improvers were assessed using a t-test. Results: At baseline, the mean age of the participants was 36.0 years and 35.7% of them were female. Participants that improved in their total AESMMI score were more likely to be female (42.9% vs 21.4%) and have at least some college education in comparison to those that did not improve (75.0% vs 46.1%, p<0.05). There was no association between races (black vs non-black). Participants who improved in their self-management practice and skills following the self-management education intervention had a higher post-intervention PIES score, indicating a reduced impact of epilepsy, compared to participants who did not improve in self-management practice. Participants who improved were also significantly more likely to have higher average self-efficacy scores post-intervention than participants who did not improve. Conclusions: This preliminary analysis highlights the success of PAUSE to improve self-management skills, but also begins to identify sub-groups that may require additional support in acquiring and applying self-management skills. Funding: PAUSE is a project supported by the University.of Illinois Prevention Research Center and the Centers for Disease Control and Prevention's MEW Network. The project is administered by the Institute for Health Research and Policy of the University of Illinois at Chicago, under CDC cooperative agreement no. U48-DP005010.