Perampanel Treatment in Refractory Status Epilepticus in a Neurological Intensive Care Unit
Abstract number :
3.303
Submission category :
7. Antiepileptic Drugs / 7C. Cohort Studies
Year :
2018
Submission ID :
509661
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Chen-Jui Ho, Chang Gung Memorial Hospital Kaohsiung Branch and Meng-Han Tsai, Chang Gung Memorial Hospital Kaohsiung Branch
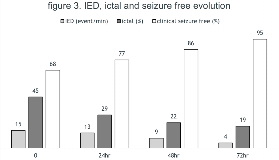
Rationale: To report the experience of a new mechanism antiepileptic drug, perampanel in refractory status epilepticus (RSE) from a neurological intensive care unit (NICU). Methods: We retrospectively collect all status epilepticus (SE) patients who received perampanel treatment admitted to our NICU. Status etiology, severity, underlying etiology and medical conditions, classifications, treatment response in EEG and clinical condition, and the short-term outcome was analyzed. Results: Total 22 patients with refractory status epilepticus who received perampanel therapy were included in this study. which account for 27.1% (22/81) of all SE. In terms of classification, 8 (36%) were generalized convulsive status epilepticus, 7 (32%) were focal to bilateral convulsive status epilepticus, 2 (9%) were focal convulsive status epilepticus, 4 (18%) were non-convulsive status epilepticus with coma, and 1 (5%) were non-convulsive status epilepticus without coma. As for etiology, 4 (18.2%) due to previous intracerebral hemorrhage with VP shunt in situ, 4 (18.2%) due to the previous trauma, 3 (13.6%) due to autoimmune encephalitis, 2 (9.1%) due to bacterial central nervous system infection, 2 (9.1%) due to arteriovenous fistula, 2 (9.1%) due to the previous ischemic stroke, 1 (4.5%) due to hydrocephalus of unknown etiology, 1 (4.5%) due to cefepime encephalopathy, 1 (4.5%) due to brain tumor and 2 (9.1%) remain unknown despite detail examinations. Among them, 13 (59.1%) received intubation and intravenous anesthesia hence fulfilled the criteria for super-refractory status epilepticus. Mean antiepileptic drugs used before perampanel was 3.4 (range:2-7, IQD:1), mean duration from onset to perampanel: 5.4 days (range 0-22, IQD 7.6). Mean baseline mRS before admission was 2.1(range: 0-5, IQD: 3.75). Mean EMSE was 86.7(range: 50-152, IQD: 48). Mean STESS was 3.2(range: 1-6, IQD: 2). Short-term outcome: 21 (95.5%) achieved 50% seizure reduction to perampanel 72 hours after treatment, 17 (77.3%) patients were both free from clinical and electrographic ictal event until the last follow. On discharge, 4 (17.4%) patients died, and average MRS was 4.8 (range 0-6, IQD: 0). Conclusions: Our preliminary findings suggest that perampanel may be an effective treatment for RSE, even in SRSE which is in accordance with previous studies. Our patient has more complex medical conditions and PER still showed adequate treatment effect in RSE and SRSE. However, this study is limited by the retrospective design and small case numbers. Further studies may be worthwhile to clarify the role of perampanel in the treatment of SE. Funding: The authors did not receive funding of this abstract.
.tmb-.png?Culture=en&sfvrsn=7ec31114_0)