Propagation Patterns of Interictal Spikes and Ripples Are Distinct: Onset Ripples Predict the Epileptogenic Zone Better Than Onset or Spread Spikes in Children with Refractory Epilepsy
Abstract number :
1.041
Submission category :
1. Basic Mechanisms / 1C. Electrophysiology/High frequency oscillations
Year :
2018
Submission ID :
501455
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Christos Papadelis, Boston Children's Hospital, Harvard Medical School; Eleonora Tamilia, Boston Children's Hospital, Harvard Medical School; Eun-Hyoung Park, Boston Children's Hospital, Harvard Medical School; Jeffrey Bolton, Boston Children's Hospital;
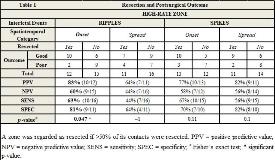
Rationale: The clinical utility of interictal spikes (1-70 Hz) to guide epilepsy surgery is hampered by their low specificity to define the epileptogenic zone (EZ). Ripples (80-250 Hz) are regarded better biomarkers than spikes, but they also have low specificity since both ripples and spikes are seen in large brain areas, whose complete resection is unnecessary for seizure freedom. A key question to be answered is how to discern ripples or spikes generated in the EZ versus those generated in normal tissue. A typical approach to estimate the EZ during the interpretation of ictal events is to distinguish between onset and spread of the epileptic activity. Here, we extend the concept of propagation to the interpretation of interictal events in both spike and ripple frequency bands. Our goal is to compare the propagation patterns of interictal spikes and ripples on intracranial electroencephalography (iEEG) of children with medically refractory epilepsy (MRE), identify their onset and spread, and evaluate whether their resection predicts surgical outcome Methods: We retrospectively analyzed iEEG, MRI, and CT data from 27 children with MRE prior to surgery. We developed an algorithm that: (i) identifies propagation sequences of ripples and spikes across neighboring iEEG contacts, combining temporal information from iEEG with spatial information from presurgical magnetic resonance imaging (MRI) and post-implantation computerized tomography (CT); (ii) calculates the latency of each propagating ripple or spike from the propagation onset; and (iii) categorizes them as either onset or spread. For each patient, we tested whether the topographic distribution of onset and spread was similar between ripples and spikes, by performing a Spearman correlation between the rates per contact of onset-ripples and onset-spikes (and similarly for spread). Finally, for both ripples and spikes, we evaluated whether the resection of the areas generating onset or spread was associated with outcome (Fisher’s test), which was dichotomized into good (Engel=1) and poor (Engel=2) Results: We found ripple propagation in all patients and spike propagation in 25 patients. Most ripple sequences (78%) did not overlap with spike sequences. The propagation latency of ripples (54 ms) was longer than spikes (16 ms; n=25, p<0.001, Wilcoxon sign-rank), while the spatial extent did not differ (6 contacts/sequence, p>
.tmb-.jpg?Culture=en&sfvrsn=cb1f2868_0)