Radiofrequency Thermocoagulation for Refractory Focal Epilepsy
Abstract number :
1.341
Submission category :
9. Surgery / 9A. Adult
Year :
2018
Submission ID :
505410
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Rebecca E. Fasano, Emory University School of Medicine; Alex Greven, Emory University School of Medicine; Katie Bullinger, Emory University; Daniel L. Drane, Emory University School of Medicine; Jon T. Willie, Emory University; and Robert E. Gross, Emory
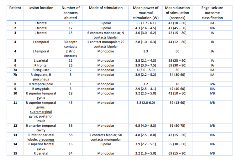
Rationale: In patients with refractory epilepsy, destructive surgery offers the chance of a cure. Radiofrequency thermocoagulation (RF-TC) is a minimally invasive technique that allows for the creation of small lesions through intracranial EEG electrodes, potentially allowing patients to avoid larger epilepsy surgeries. We describe a series of 16 patients who underwent RF-TC of depth and/or strip electrode contacts. Methods: Between 1/14 and 5/17, 15 patients with refractory focal epilepsy underwent sEEG and RF-TC at our comprehensive epilepsy center. Patients were treated with RF-TC after intracranial seizure localization. RF-TC was chosen due to location of the seizure focus in eloquent cortex or as a preliminary treatment in hopes of avoiding a larger epilepsy surgery. Electrode contacts involved in seizure onset and early spread were ablated using a radiofrequency lesion-generator system (Cosman Medical Inc., Burlington, MA, USA). In patients with seizure foci in eloquent cortex, neurologic function was tested before and after each increase in power. EEG was recorded before and after ablation. Brain MRI was performed within 24 h to determine lesion adequacy. Seizure outcomes and neurologic deficits were assessed postoperatively. Results: 15 patients were included (10 female, 5 male); the median age was 43 (range 22-60) yrs. 6 pts were lesional (3 focal cortical dysplasias; 1 remote astrocytoma resection; 1 cystic lesion; 1 encephalomalacia); 9 were non-lesional. sEEG onsets were lateralized to the R in 10 pts and to the L in 5. Localization was temporal (6), frontal (6), parietal (1), and cingulate (1); 3 pts had multifocal onsets. Six patients underwent RF-TC due to onsets in eloquent cortex. Nine patients underwent RF-TC as a “test ablation” procedure to avoid a larger surgery. All patients underwent RF-TC while awake, at the bedside (11 pts) or in the OR (4 pts). Current was delivered stepwise from 1.5 to 8 W for up to 90 s. A median of 16 (range 1-58) depth electrode contacts were ablated. Two strip electrode contacts were ablated in 1 patient. Re-ablation was performed in 3 patients who had continued epileptiform activity or seizures post-ablation. One patient in the eloquent cortex group underwent immediate laser ablation due to inadequate lesion size on post-procedure MRI. Four of 6 patients with eloquent cortex onsets were Engel Class IA/IB at a median of 24 (range 19-40) months postop. No patient in the “test ablation” group was Engel Class IA/IB; 1 was Class IIA; and 8 were Class III/IV at a median of 13 (range 10-16) mths postop. Lesional patients also had better outcomes (66% Engel Class IA/IB) vs. non-lesional (22% Engel Class IA/IB). One pt developed an intraparenchymal hemorrhage postop with transient hemiparesis; one patient had persistent hemifacial numbness. Eight patients (one in the eloquent cortex group) ultimately underwent laser ablation or open resection for continued seizures. Conclusions: RF-TC is a safe, minimally invasive treatment option for patients with refractory focal epilepsy. Patients who underwent RF ablation of seizure foci in eloquent cortex had better outcomes. Patients who underwent RF ablation to avoid larger surgery had poorer outcomes; 78% ended up undergoing laser ablation or open resection due to continued seizures. Longer follow-up and larger series are needed to confirm the efficacy of this procedure. Funding: None