Resting state fMRI and Epilepsy Surgery : A Pilot Study in Children
Abstract number :
1.354
Submission category :
9. Surgery / 9B. Pediatrics
Year :
2018
Submission ID :
506995
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Henry Osso-Rivera, Nicklaus Children's Hospital; Marytery Fajardo, Nicklaus Children's Hospital; Byron Bernal, Nicklaus Children's Hospital; Magno Guillen, Nicklaus Children's Hospital; and Ann Hyslop, Nicklaus Children's Hospital
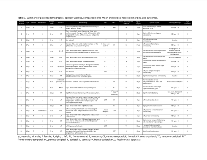
Rationale: Resting state fMRI (rs-fMRI) consists of a sequence of several time points sensitive to minute changes in blood oxygen regional changes. Prior publication from our group has shown differences between normal subjects and epilepsy patients on the average of these time points (rs-mean). We aimed to ascertain the potential role of rs-mean in epilepsy focus localization and its value in prognosis. Methods: Twenty children with medically refractory epilepsy who had rs-fMRI and underwent epilepsy surgery from 2009 through 2015 at Nicklaus Children’s Hospital were included in this pilot study. All cases were seizure free for at least two years post-operatively. Patients with tumors were excluded. Pre-operative rs-mean volumes were color coded and co-registered to the post-operative axial T1 MRI using Mango software. Two independent blind raters identified the presence of local mean hyperintensity (LMH) and evaluated the degree of overlap between the LMH and the resected tissue. Six grades were identified: (I) LMH located in the contralateral hemisphere of resection or absent; (II) no overlap but the LMH located in a different lobe of the ipsilateral hemisphere; (III) no overlap but LMH located in the same lobe; (IV) overlap of any type with resection isocenter outside of LMH; (V) overlap of any type with resection isocenter inside LMH; and (VI) overlap with resection isocenter inside the main LMH. Disagreements between raters were resolved by consensus. Demographic and neuroimaging variables were annotated. Results: Table 1 summarizes the demographics and primary measures studied, which include grade of overlap of resection margins with rs-mean, EEG, MRI, PET, and SPECT findings, etiology, duration of epilepsy, and seizure outcomes. Mean age of seizure onset of 6.3 years (range: 2-13 years). The mean age for epilepsy surgery was 10.9 years (range: 3-19 years). Types of surgery included corticectomy (n=11), thermal ablation (n=4), lobectomy (n=4), and tuberectomy (n=1).In 25% of cases (n=5) the LMH was either not present or in the contralateral hemisphere, in 20% of cases (N=4) the LMH was in the ipsilateral hemisphere without overlap with the resection margins, and in 55% of cases (n=11) there was overlap between the LMH and the resection margins. Conclusions: In more than half of our cohort, there was overlap noted between the surgical resection and the LMH. This preliminary data suggests rs-mean may be a potentially beneficial non-invasive tool in presurgical evaluation, particularly in complex cases without identified lesions or with multiple regions of interest (e.g., tuberous sclerosis), though further research is needed. Analysis of a larger cohort and subgroups, including those based on neuroimaging findings, etiology, and duration of epilepsy, will be performed to understand whether rs-mean may be helpful in the evaluation of patients with certain characteristics. Funding: None