Stereotactic Laser Ablation for Neocortical Epilepsy
Abstract number :
3.326
Submission category :
9. Surgery / 9A. Adult
Year :
2018
Submission ID :
500745
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Paul Koch, Emory University; Supriya Ramesha, Emory University; Daniel Graf, Emory University; Brian Cabaniss, Emory University; Robert E. Gross, Emory University School of Medicine; and Jon T. Willie, Emory University
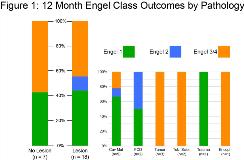
Rationale: Laser interstitial thermal therapy (stereotactic laser ablation, SLA) has emerged as an effective minimally invasive therapy for medically refractory medial temporal lobe epilepsy while offering an improved neurocognitive risk profile relative to open resection. Although SLA has also been reported to successfully treat hypothalamic hamartomas, tubers, and focal cortical dysplasias, especially in the pediatric population, there are no large series describing outcomes of SLA for adult neocortical epilepsy. In a systematic review and meta-analysis, seizure free outcomes from open resection for refractory neocortical epilepsy ranged widely from 34% in non-lesional cases to 66% in lesional cases. We present here our experience using MRI-guided SLA of the neocortex for the treatment of medically refractory epilepsy with and without structural lesions. Methods: We retrospectively reviewed the surgical outcomes of all patients who underwent MRI-guided SLA of any cortical focus outside the medial temporal lobe for the treatment of medically refractory epilepsy at Emory University with at least 12 months of follow-up. Results: Twenty-five patients were identified who underwent neocortical SLA between 2012 and 2017 (15 [60%] female, mean age 38 [+/- 17.4 SD, range: 18-77] years). Patients had follow-up data out to a mean of 28.3 (+/- 13.9 SD, range: 12-57) months. Seven (28%) patients had no structural lesion identified on imaging, of which 6 (85.7%) underwent intracranial monitoring prior to ablation. Of the 18 (72%) patients with identified, targeted lesions, 9 (36%) had cavernous malformations, 3 (12%) had low grade tumors, 2 (8%) had focal cortical dysplasias, 2 (8%) had tuberous sclerosis, 1 (4%) had an encephalocele and 1 (4%) had post-traumatic gliosis. Eight (44.4%) lesion patients underwent intracranial monitoring prior to ablation. At 12 months post-SLA, 44.0% (95% CI 26.7-63.0%) were Engel class 1 (free of disabling seizures ), 8.0% (95% CI 1.4-25.0%) were Engel class 2 and 48.0% (95% CI 30.0-66.5%) were Engel class 3 or 4. 42.9% (95% CI 15.8-75.0%) of non-lesional patients and 44.0% (95% CI 24.6-66.3%) of lesional patients were Engel class 1 at 12 months. Figure 1 presents 12 month outcomes by lesion type. Figure 2 presents Kaplan-Meier curves of seizure freedom (Engel class 1) for the total cohort and the subgroups with and without structural lesions, demonstrating that seizure freedom rates are stable beyond 13 months to over 3 years. Complications (a cranial nerve 7 palsy, a temporary weakness of face and arm, and a small asymptomatic hemorrhage) were observed in 3 patients. Mean hospital length of stay post-SLA was 1.3 (+/- 0.68 SD, range: 1-4) days with no 30-day readmissions. Conclusions: Our data suggest that SLA for neocortical focal epilepsy is effective, safe and well-tolerated. We achieved 43% and 44% seizure freedom at 12 months in lesional and non-lesional patients, respectively. In the case of non-lesional patients, these outcomes are consistent with those reported after open resection, while our outcomes in the case of lesional patients may be lower. However, many patients were initially unwilling to undergo open resection. SLA provides a reasonable chance of seizure freedom with little surgical risk and it raises little or no barrier to subsequent procedures such as intracranial monitoring, further ablation, or open surgery, enabling an iterative surgical approach to focal epilepsy. SLA represents a paradigm shift towards more minimally invasive yet effective epilepsy surgery. Funding: None
.tmb-.jpg?Culture=en&sfvrsn=fbd65046_0)