The Risk of New-Onset Epilepsy and Pharmacologically Refractory Epilepsy in Older Adult Stroke Survivors
Abstract number :
1.427
Submission category :
16. Epidemiology
Year :
2018
Submission ID :
496251
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Tresah C. Antaya, Western University; Jorge G. Burneo, Western University; Britney N. Allen, Institute for Clinical Evaluative Sciences Western; Andrea Belisle, Institute for Clinical Evaluative Sciences Western; Salimah Z. Shariff, Institute for Clinical
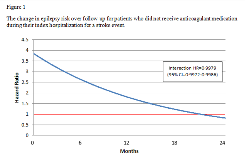
Rationale: Despite stroke being a common cause of new-onset epilepsy in older adults, stroke-related epilepsy has rarely been studied in this population. Methods: We conducted a population-based, retrospective cohort study using linked, administrative healthcare databases. The Ontario Stroke Registry was used to identify patients 67 years and older who were hospitalized for a stroke at a designated stroke centre in Ontario, Canada between April 1, 2003 and March 31, 2009, and were previously free of epilepsy. Multivariable Fine-Gray hazard models were used to examine risk factors of new-onset epilepsy and refractory epilepsy, accounting for the competing risk of death. Five-year mortality and the receipt of diagnostic care were evaluated for those who developed epilepsy. Results: Among 19,138 older adults hospitalized for a stroke, 210 (1.1%) developed epilepsy and 27 (12.9%) became refractory to antiepileptic drugs. Within one year of epilepsy diagnosis, 24 (11.4%) patients were assessed with electroencephalography (EEG) and 19 (9.0%) with magnetic resonance imaging (MRI). In multivariable analysis, age was a significant risk factor of both epilepsy (HR=0.91, 95% CI=0.88 – 0.93) and refractory epilepsy (HR=0.89, 95% CI=0.82 – 0.98). Female sex also increased risk of epilepsy (HR=1.60, 95% CI=1.13 – 2.27) and refractory epilepsy (HR=2.91, 95% CI=1.02 – 8.29). The effects of not receiving anticoagulant medication in hospital initially increased epilepsy risk (HR=3.84, 95% CI=1.79 – 8.27), however this effect decreased over time (HR=0.9979, 95% CI=0.9972 – 0.9986), crossing the point of equivalent risk (Figure 1). Similarly, having a higher Canadian Neurological Scale score initially increased epilepsy risk (HR=1.15, 95% CI=1.08 – 1.23), but this effect also decreased over time (HR=0.9997, 95% CI=0.9996 – 0.9997) (Figure 2). In the five years following epilepsy diagnosis, 97 (46.2%) participants died of any cause, 13 (6.2%) of stroke-related causes, and none of epilepsy-related causes. Conclusions: We found that risk of both stroke-related epilepsy and refractory epilepsy decreases with age. Biologically, these phenomena can be explained by decreasing neuronal plasticity and metabolism over the lifespan. We also found that our study sample, on average, did not receive the neurodiagnostic tests that are recommended by current guidelines. Therefore, these patients may have additional undetected epileptogenic lesions. We also found that most deaths among those who developed epilepsy were not attributed to either stroke or epilepsy. These findings have important implications for the clinical management of older adults who develop new-onset epilepsy following a stroke. Funding: Ontario’s Ministry of Health and Long-Term Care, the Academic Medical Organization of Southwestern Ontario, Western University’s Schulich School of Medicine and Dentistry, Lawson Health Research Institute, and the Canadian Institutes of Health Research.
.tmb-.png?Culture=en&sfvrsn=2db77af5_0)