Utilization of a Standardized Discharge Template Is Associated With Lower 30-Day Readmission Among Pediatric Patients With Seizures
Abstract number :
1.411
Submission category :
13. Health Services (Delivery of Care, Access to Care, Health Care Models)
Year :
2018
Submission ID :
502512
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Jaspreet Benwait, Boston Children's Hospital; Jennifer Nguyen, Boston Children's Hospital, Harvard Medical School; Madeline Chiujdea, Boston Children's Hospital; Annalee Antonetty, Boston Children's Hospital; and Jamie Heath, Boston Children's Hospital, H
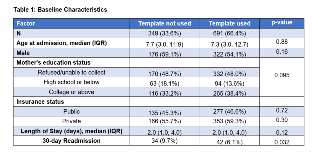
Rationale: As healthcare evolves, there is an increasing drive to provide high quality care at lower cost. A key quality measure that addresses this goal is the rate of preventable readmissions. As preventability is difficult to assess and varies across specialties, providers and institutions, a common surrogate measure is unplanned readmissions. In 2015, our department assembled a taskforce to address unplanned readmissions and has implemented multiple interventions to decrease unplanned readmission rates. Seizures account for the leading cause of hospital readmissions among our patient population in the inpatient pediatric neurology services at our institution. In this study, we aim to assess the effect of a standardized discharge template on 30-day readmission rates in the pediatric inpatient epilepsy service at a large tertiary care academic center. Methods: Using an internal data warehouse, all unplanned readmissions to the inpatient epilepsy service were identified within our tertiary care referral medical center from May 2016 to December 2017. A standardized discharge template was created and implemented in May 2016 consisting of 3 key components including patient diagnosis, phone number to call with questions or concerns, and seizure action plan. Residents and nurse practitioners were trained on appropriate template use. Template utilization was verified by chart review on a monthly basis. Readmission within 30 days of discharge was identified by reviewing encounter level data group. Logistic regression modeling was performed to calculate odds of readmission and adjust for baseline characteristics. Results: The cohort consisted of 1040 patients, with a median age of 7.5 years, 44.2% female. The discharge template utilization rate was 66.4%. The readmission rate within 30-days of discharge over this time period was 7.3%. There were no significant differences in baseline characteristics when comparing patients who received a standardized discharge template compared to those who did not (Table). However, there was a significant reduction in unplanned readmission rates when comparing the two groups (6.1% vs 9.7%; p=0.03). There was also a significantly lower odds of readmission for the discharge template group (unadjusted OR=0.60, p=0.03) that remained unchanged after adjustment for baseline characteristics (OR = 0.59, p=0.04). Additionally, younger patient age was a significant independent predictor of 30-day readmission (adjusted OR=0.94, p=0.004; per 1-year increase in age). Conclusions: The use of a standardized discharge template was associated with a 40% reduction in the odds of readmission within 30-days of discharge among pediatric patients admitted to the epilepsy service. Use of the template may also have improved parental education at discharge potentially contributing to lower readmission rates. Limitations of this study include residual confounding due to unmeasured confounders. Further studies are needed to assess the large-scale feasibility and efficacy of this intervention and its potential role in EMR integration. Funding: No funding was received in support of this abstract.