Widespread Alterations in Functional Connectome Embedding Following Temporal Lobe Epilepsy Surgery
Abstract number :
2.190
Submission category :
5. Neuro Imaging / 5B. Functional Imaging
Year :
2018
Submission ID :
501194
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Sara Lariviere, Multimodal Imaging and Connectome Analysis Lab, McConnell Brain Imaging Centre; Yifei Wang, Nanjing Drum Tower Hospital; Reinder Vos de Wael, Multimodal Imaging and Connectome Analysis Lab, McConnell Brain Imaging Centre; Zhengge Wang, Nan
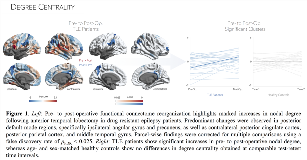
Rationale: Temporal lobe epilepsy (TLE) is the most common drug-resistant epilepsy in adults. Resective temporal lobe surgery is currently the most effective treatment to control the seizures. Despite its high clinical utility, the downstream consequences of this invasive procedure on large-scale functional networks remain to be established. In the current study, we longitudinally assessed pre- to post-operative functional connectome reorganization in a cohort of TLE patients. Methods: We obtained pre- and post-operative (at least 1 year follow-up) structural and resting-state functional MRI from 30 drug-resistant unilateral TLE patients admitted to Jingling Hospital (14 males; 27.2±8.6 years; Engel I/II-IV=19/11). Neuroimaging data from 26 age- and sex-matched controls, scanned at comparable time intervals, were also acquired. Patients underwent anterior temporal lobectomy between both time points, and post-operative histopathology revealed hippocampal sclerosis in every patient. We mapped resting-state fMRI time-series onto each subject’s cortical surface and correlated the time series between each regional pair to derive individualized functional connectomes. The z-transformed connectomes were thresholded to retain only the top 10% of weighted connections for each region. To avoid bias in network size, we excluded the surgical lacuna in both pre- and post-operative matrices. Following the normalization of features against corresponding control networks, data from TLE patients were sorted into ipsilateral/contralateral to the seizure focus. We computed nodal degree centrality, indexing the connectome embedding of a given region. Linear mixed-effect models tracked (i) pre- to post-operative network changes in TLE patients and (ii) test-retest reliability in controls. Findings were corrected for multiple comparisons using a false discovery rate (FDR) of pFDR < 0.025. Results: Comparing pre- to post-operative time points in TLE patients, we observed marked reorganization in functional network topology, specifically post-operative increases in degree centrality in default-mode regions, including ipsilateral precuneus, angular gyrus, as well as contralateral posterior cingulate cortex, posterior parietal cortex, and middle temporal gyrus (Figure 1). Comparing baseline and follow-up centrality in our healthy controls during an equivalent interval, we did not observe significant changes. Notably, post-hoc interaction analysis in regions of patient-specific centrality increases revealed more marked increases in patients compared to controls (pFDR < 0.025), suggesting that surgery-induced network organization goes above and beyond test-retest intervals. Conclusions: Our analysis revealed post-operative functional connectivity changes across a broad and diffuse territory, which nevertheless appears to be preferentially co-localized within default-mode network, suggesting anatomical constraints on post-operative functional remodeling. Future studies are needed, however, to clarify co-occurring structural changes and associations to post-surgical outcome. Funding: CIHR, SickKids Foundation, NSFC, FRQS